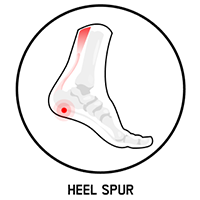
Confirmed by radiographic findings at the pain location. As many as 50% of patients with plantar fasciopathy have heel spurs. A heel spur is usually an incidental finding that is not diagnosed on the basis of the patient’s symptoms [1,3].
You are here
01 - Assess & engage
SEE ALL
CHAPTERS
The patient’s history, together with the physical examination of the foot and ankle, should provide valuable insights regarding the underlying pathology. Common red flags include:
Although plantar fasciopathy is the most common source of plantar heel pain, the differential diagnosis of plantar fasciopathy is broad, encompassing arthritic conditions, infections, neuropathies, and mechanical causes. Mechanical etiologies of plantar heel pain include:

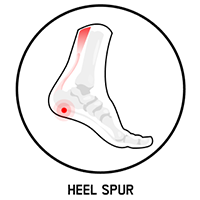
Confirmed by radiographic findings at the pain location. As many as 50% of patients with plantar fasciopathy have heel spurs. A heel spur is usually an incidental finding that is not diagnosed on the basis of the patient’s symptoms [1,3].
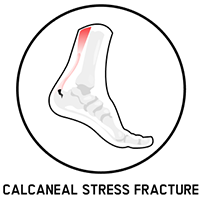
Pain during activity, progressing to pain at rest.
(medial or lateral plantar nerve, nerve to abductor digiti minimi). Characterized by feelings of burning, tingling, or numbness.
manifested by deep, bruise-like pain, is typically localized in the middle of the heel.

manifested by a sensation of pain, burning and tingling on the sole of the foot.
The treatment of plantar fasciopathy and the alleviation of pain to increase the patient’s quality of life requires:
The treatment of plantar fasciopathy can include pharmaceutical and non-pharmaceutical methods such as Guided DolorClast® Therapy. It is recommended to begin the therapy with a non-pharmacological and non-invasive approach, such as shock wave therapy, physical exercise, and patient education, before pharmacological interventions. Opioids and steroids may reduce pain and inflammation, but they do not improve function and are associated with side effects, such as nausea and headache.
Pain can have multiple origins, such as mechanical strain, degeneration of tissues, inflammation, and edema. The tendency is often to treat the dominant symptom – in this case, pain – without resolving its cause. With quick fixes such as painkillers, underlying inflammation can be neglected, preventing tissue healing. Although the patient may be satisfied with the recession of pain, this may ultimately lead to greater damage due to the stress that continues to be applied to the injury. Compared to other approaches, radial shock waves effectively reduce pain and inflammation with no side effects.
As many as 20% of plantar fasciopathy patients experience persistent symptoms and unsatisfactory treatment outcomes [5-6]. A recent meta-analysis comparing as many as seven different treatment modalities in plantar fasciopathy patients concluded that RSWT® offered more effective and stable pain relief compared with other interventions [5].
Copyright © 2024 EMS DolorClast